A yeast infection is a common vaginal infection caused by an overgrowth of a type of yeast called Candida. It often leads to itching, irritation, and unusual discharge. A yeast infection can happen for many reasons, but certain risk factors can increase your chances of developing one.
If you’ve ever experienced a yeast infection, then you understand the discomfort and frustration it causes. Unfortunately, most women won’t get only one yeast infection in their lifetime. Yeast infections can be a frequent or even a chronic problem that interferes with everyday life.
3 out of 4 women will get one or more yeast infections in their lifetime, making them one of the most common vaginal infections.
But there are other types of vaginosis, such as bacterial vaginosis (BV), that are just as common, and many yeast infection symptoms can be similar to signs of BV or even certain sexually transmitted infections (STIs).
That overlap can lead to misdiagnosis, delayed treatment, and recurring infections.
Whether this is your first yeast infection and you aren’t sure if the symptoms you’re having line up with a yeast infection or are signs of BV, or you’ve had a yeast infection before and it’s come back again, it’s important to fully understand what a yeast infection is, what causes them, what your symptoms might be telling you about your vaginal health and when it’s time to stop guessing and see an OB-GYN.
In this article, we’ll walk through what a yeast infection is, what causes it, the most telling symptoms of a yeast infection, and if you can treat a yeast infection at home or if it’s a better idea to see a gynecologist in Tennessee.
What is a Yeast Infection?
A yeast infection, also known as candidiasis, is a common vaginal infection caused by an overgrowth of a fungus. Unlike many infections that are caused by bacteria or viruses, a yeast infection is one of the few that develops due to a fungal imbalance.
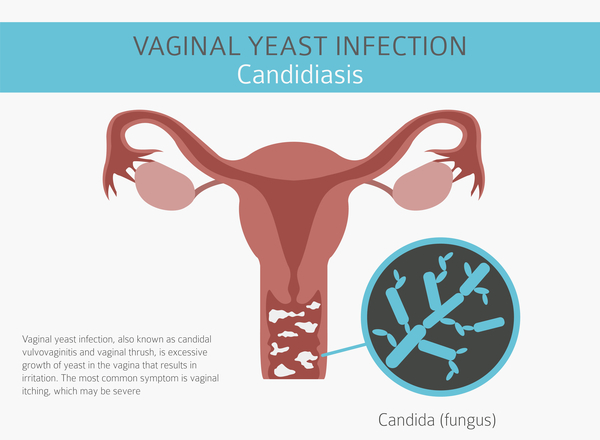
This fungus, called Candida albicans, is a naturally occurring microorganism that lives in the vagina alongside healthy bacteria. Normally, everything stays in balance. But when that balance is disrupted, Candida can multiply rapidly, leading to uncomfortable symptoms.
While some yeast in the body is normal, certain triggers like antibiotics, hormonal changes, or even tight clothing can throw off the vaginal microbiome and lead to a yeast infection.
Yeast infections aren’t usually serious, but they shouldn’t be ignored. Without proper treatment, symptoms can worsen or recur, so it’s important to address them early for fast relief and to prevent complications.
What Causes a Yeast Infection?
There are many reasons why Candida can multiply and lead to a yeast infection. The most common triggers include taking antibiotics or experiencing hormonal shifts during pregnancy.
However, those aren’t the only causes. Other factors, like a weakened immune system, poor hygiene, or chronic health conditions, can also increase your risk of developing a yeast infection.
Here’s a closer look at what can cause or increase your risk of getting a yeast infection and why:
Taking Antibiotics
Antibiotics kill both bad and good bacteria in the body. When the helpful bacteria in your vagina are wiped out, it gives yeast a chance to grow unchecked.
Pregnancy
Hormonal changes during pregnancy (especially increases in estrogen) can create the perfect environment for yeast to multiply.
Poor Hygiene Practices
Overwashing, using scented soaps or douches, or wearing damp underwear or other tight clothing can disrupt your natural pH and allow yeast to thrive.
Sexual Contact
While yeast infections aren’t classified as sexually transmitted infections (STIs), they can be passed between partners during sexual contact, especially if left untreated.
General Hormone Imbalances
Hormone disorders or hormone fluctuations from birth control, your menstrual cycle, or menopause can upset the balance of bacteria and yeast in the vagina.
A Weakened Immune System
If your immune system is compromised due to illness or medication, your body may not be able to keep yeast levels in check.
Chronic Conditions (Such As Diabetes)
High blood sugar levels (especially when poorly managed) can feed yeast and increase your chances of infection.
A Poor Diet
Diets extremely high in processed sugar, refined carbs, or processed foods can contribute to yeast overgrowth in the body.
Sleep Deprivation
Lack of rest can weaken the immune system and increase stress hormones, which may trigger or worsen infections.
Foreign Objects
There are many things that you should never put in your vagina that can lead to problems, including yeast infections.
However, even items that are made for vaginal use, such as tampons, menstrual cups, or contraceptive devices, can cause issues if left in too long. These products can create a warm, moist environment where yeast thrives, increasing the risk of infection.
Symptoms of a Yeast Infection
If yeast cells begin to multiply in the vagina, it can trigger a range of uncomfortable and unpleasant symptoms. The most common signs women experience are itching and an abnormal vaginal discharge that is typically thick, white, and odorless.
Yeast infection symptoms can appear suddenly or come about more slowly. Regardless of onset, if you have a common yeast infection, you will likely have one or more of the following symptoms:
- Itching and irritation in the vagina and vulva (vaginal opening)
- Thick, white, odorless vaginal discharge (often, but not always described as a cottage cheese texture)
- Redness, swelling, or inflammation of the vulva
- A burning sensation, especially during urination or intercourse
- Vaginal pain or soreness
These symptoms can range from quite severe to extremely mild. In fact, some women (especially those experiencing their first yeast infection) may have such mild symptoms that they go unnoticed or seem to resolve on their own, not realizing they have a yeast overgrowth until the infection advances.
If this happens, it may be considered a complicated yeast infection. In these cases, the common symptoms listed above are typically much more intense. You might even experience tears, cracks, or sores in the vagina.
A complicated yeast infection can happen to anyone, but is more likely to occur if:
- You experience four or more yeast infections in a single year (recurrent infections)
- Your infection is caused by a less common type of yeast, such as Candida glabrata, instead of Candida albicans
- You are pregnant
- You have uncontrolled diabetes
- You have a weakened immune system due to a medical condition (such as HIV/AIDS) or medications (such as chemotherapy or long-term corticosteroids)
Some women also develop complicated infections because they mistake the symptoms for another type of vaginal infection and delay proper treatment (the most common being bacterial vaginosis, which we will discuss next.)
If you’re unsure whether your symptoms are caused by a yeast infection or something else, it’s important to get a proper diagnosis from a gynecologist. Identifying the right infection early means faster relief and fewer chances of it coming back.
Yeast Infection vs. Bacterial Vaginosis: How to Tell the Difference
Yeast infections and bacterial vaginosis (BV) are two of the most common vaginal infections. They are frequently confused with one another, but they’re caused by entirely different organisms and require different treatments.
In most cases, it’s fairly easy to distinguish a yeast infection from other types of vaginosis, such as BV, based on discharge and odor. For example, BV typically causes a thin, watery discharge with a strong fishy smell, which is very different from the thick, odorless discharge seen in most yeast infections.
Still, symptoms don’t always present clearly. Early signs like itching, discomfort, and inflammation can overlap with BV or even other types of infections, making self-diagnosis tricky.
Here are the key differences between bacterial vaginosis and a yeast infection, and why a proper diagnosis matters:
Yeast Infections and BV Have Different Underlying Causes
A yeast infection is caused by an overgrowth of Candida (a fungus), while BV is caused by an imbalance in vaginal bacteria, typically a decrease in beneficial lactobacilli and an overgrowth of harmful bacteria.
Bacterial vaginosis is the most common type of vaginal infection in women aged 15 to 44. The primary causes are bacterial imbalances from douching and sex, but it’s not a fungal infection like you would typically get with a yeast infection.
Key Differences in Yeast Infection and BV Symptoms
One of the most noticeable differences between yeast infections and bacterial vaginosis is the odor and discharge consistency.
Yeast infections typically produce a thick, white, odorless discharge that resembles cottage cheese. Bacterial vaginosis usually causes a thin, watery, gray, or white discharge (sometimes with an “egg white” consistency) that often has a strong fishy odor, especially after sex.
Bacterial vaginosis also doesn’t usually cause the same level of itching or redness associated with a yeast infection. With a yeast infection, itching and irritation can be intense, sometimes accompanied by swelling and redness around the vulva.
With bacterial vaginosis, any itching around sensitive areas like the labia minora or clitoral hood is generally mild. Instead, you’re more likely to experience a burning sensation, particularly during urination or intercourse.
Why Getting The Right Diagnosis Matters
Getting the right diagnosis from a gynecologist matters because the treatments for a yeast infection are very different from bacterial vaginosis treatment.
Yeast infections are typically treated with antifungal medications, either over-the-counter or prescription. Bacterial vaginosis, on the other hand, typically requires a prescription antibiotic, such as metronidazole or clindamycin. Treating bacterial vaginosis with an antifungal won’t help, and vice versa.
Bacterial vaginosis is tough to identify and can cause long-term complications if left untreated. If you suspect you have bacterial vaginosis, you will need to visit your gynecologist in Tennessee for an antibiotic prescription in order to clear up BV.
Additionally, early signs like itching, discomfort, inflammation, and unusual discharge can also overlap with a sexually transmitted disease (STD) or sexually transmitted infection (STI) such as trichomoniasis, chlamydia, gonorrhea, or herpes.
Because yeast infections can sometimes share overlapping symptoms with other infections and because untreated BV can lead to complications like increased risk of STIs or pregnancy issues, it’s important to get tested if you’re unsure.
Yes, there are over-the-counter yeast infection tests and pH tests that may give you a general idea of what type of infection you might have. However, only a healthcare provider can accurately determine the cause and recommend the proper treatment for faster, more effective relief.
Diagnosing and Treating a Yeast Infection
Many women attempt to self-diagnose and self-treat a vaginal infection, especially if it’s their first one. Often, this is because most women believe vaginal infections aren’t serious and don’t warrant a visit to the doctor.
It is true that yeast infections aren’t dangerous, but they can be easily mistaken for other conditions, like bacterial vaginosis or an STI. This delays proper treatment and can prolong symptoms, potentially leading to complications like increased irritation, vaginal fissures, or spreading of the fungal overgrowth.
Another reason some women hesitate to seek medical help is out of fear, embarrassment, or shame. We understand that a yeast infection may seem worrisome or even uncomfortable to talk about, especially if you’ve never had one. However, it’s important to remember that yeast infections are common and nothing to be ashamed of.
Approximately 75% of women will experience a yeast infection at some point in their lives. Still, despite their prevalence, it’s important to treat vaginal yeast infections early.
Early treatment not only brings fast relief but also helps prevent more stubborn infections and lessens the risk of recurrence. Your gynecologist can also help you identify any underlying causes and explore preventive options.
So, whether it’s your first assumed yeast infection or you experience recurrent yeast infections (defined as four or more per year), it’s always a good idea to visit your doctor for a proper diagnosis and to rule out other possible causes, such as bacterial vaginosis or a sexually transmitted infection.
How a Yeast Infection is Diagnosed
Confirming your yeast infection diagnosis is usually very straightforward. Your doctor will typically begin with a discussion about your symptoms and medical history. Then, during a pelvic exam, they may inspect the vaginal area for signs of irritation, discharge, or inflammation.
To confirm the diagnosis, your provider may take a small sample of vaginal discharge using a sterile swab. This sample is examined under a microscope or sent to a lab to identify the presence of Candida, the fungus responsible for yeast infections.
In some cases, a culture test may be performed to determine the exact species of yeast, especially if you’re experiencing recurrent or treatment-resistant infections.
How Yeast Infections are Treated
Once you’ve been properly diagnosed with a yeast infection, there are several treatment options. Remedies for vaginal yeast infections are now easier than ever, and in most cases, the infection resolves quickly.
For uncomplicated yeast infections, your doctor will usually suggest an over-the-counter antifungal cream, ointment, or suppository. These treatments are available in 1-, 3-, and 7-day regimens depending on the brand and severity of symptoms.
Common over-the-counter options include:
- Butoconazole (Gynazole)
- Clotrimazole (Lotrimin)
- Miconazole (Monistat)
- Terconazole (Terazol)
Most uncomplicated yeast infections begin to clear up within a few days of starting OTC treatment. However, if symptoms persist beyond a week, worsen, or return soon after, follow up with your provider.
For more severe or complicated yeast infections, your gynecologist may recommend a longer course of OTC treatment or prescribe something stronger, like prescription oral antifungal medication.
Common prescription antifungal medications include:
- Fluconazole (Diflucan)
- Itraconazole (Sporanox)
Your doctor may prescribe these oral medications alongside or in place of over-the-counter treatments. Most treatments take a few days on average, but in more severe cases, it may take up to two weeks before symptoms subside.
How To Prevent a Yeast Infection (Vaginal Candidiasis)
While it might not be possible to prevent a yeast infection, there are several simple precautions and preventative measures you can take to help lower your risk.
For starters, most doctors recommend avoiding douching and scented feminine products (like pads or tampons) because these items can change the natural balance of bacteria and yeast in the vagina, potentially leading to a yeast infection.
When it comes to douching, remember that the vagina is a self-cleaning organ. Douching is not only unnecessary for most women, but it can also do more harm than good by disturbing the vaginal microbiome.
It is also advised not to wear tight, non-breathable clothing or stay in sweaty or wet clothing, like swimsuits or workout gear, for extended periods of time. This is true any season, but summers in Tennessee can get exceptionally hot and humid and further increase your risk, especially if you remain in damp swimwear after swimming.
And while it may go without saying, never share undergarments or swimwear, as this can introduce new bacteria and affect your vaginal balance. Also, during sexual activity, always practice good hygiene. Washing your hands and sex toys before and after use, using condoms, and urinating after intercourse can all help reduce the risk of introducing or spreading bacteria that may disrupt the vaginal environment.
You might also want to think twice about taking antibiotics. While antibiotics are sometimes necessary to relieve some types of infections, they kill off good bacteria as well. This can wipe out the “good” bacteria that help keep vaginal yeast in check. Without these protective bacteria, yeast can multiply rapidly and lead to an infection. The careful balance of good bacteria is what keeps the vagina healthy and fungal Candida away.
When to See a Gynecologist in Brentwood, Tennessee
We understand that it can be embarrassing to discuss things like feminine odor with anyone, even an OBGYN. However, if you are experiencing itching, discomfort and an unusual discharge, do not wait to see a gynecologist to confirm that your symptoms are actually a yeast infection and not another common vaginal infection.
Treatment for a yeast infection and other types of vaginosis are usually very simple and provide relief in as little as a few days.
There’s no need to feel uncomfortable any longer! If you are experiencing any of the following, it’s time to give us a call:
- This is the first time you have had any signs of a vaginal infection
- You are not sure what type of infection you may have
- Over-the-counter vaginal antifungal products aren’t working
- Your symptoms worsen, or you develop more
Get a yeast infection diagnosis and relief today! Call to schedule your appointment with one of the OB/GYNs in Brentwood and Cool Springs, Tennessee.

