Genital warts, also known as condyloma acuminatum, are one of the most common sexually transmitted infections (STIs) in both men and women. Genital warts are caused by certain strains of the human papillomavirus (HPV). They can be passed through any skin-to-skin sexual contact with a person who is infected.
Genital warts often have no symptoms, so it’s possible to have them without realizing it. If symptoms of genital warts do appear, they usually look like small, flesh-colored or red bumps on the butt or surrounding areas. Sometimes genital warts hurt or itch, while other times they cause no discomfort.
This leads many women to mistake female genital warts for irritation, razor bumps, or another harmless skin change. Other women might see a genital bump and worry that it could be another STI, such as herpes or syphilis. While these sexually transmitted infections can cause bumps or sores around the genitals, they have distinct visual differences and other symptoms.
It is important to know about female genital warts because they are a common sexually transmitted infection that many women are unaware of or do not fully understand. Left untreated, genital warts can spread or worsen over time.
Early detection, proper diagnosis, and treatment are essential for preventing further complications and reducing the risk of transmission to others.
What Are Female Genital Warts?
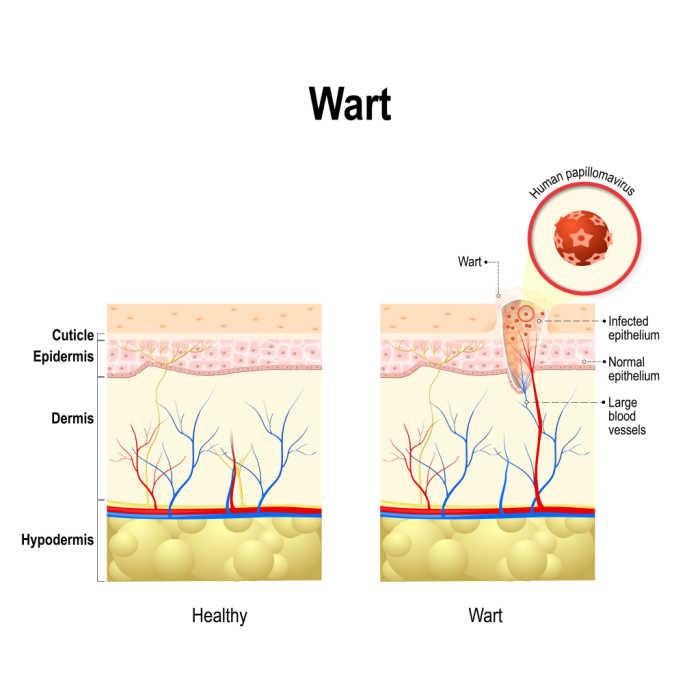
“Wart” is a common term used to describe a small growth or bump on the skin. Warts can appear anywhere on the body and are all caused by a type of virus called human papillomavirus (or HPV). However, not all warts cause genital warts. Where warts appear depends on the HPV strain and how they were transmitted, and it’s typically very easy to tell the difference between a genital wart and other skin warts.
Skin warts, such as common warts or plantar warts, do not appear on the genitals. They show up on other areas of the body, such as the hands, fingers, feet, or around, and sometimes even in the mouth. They are not sexually transmitted and are usually passed by direct contact with contaminated surfaces or through small breaks in the skin.
Genital warts appear in the genital and surrounding areas and are sexually transmitted. You cannot get genital warts from kissing or from sharing things like cups and utensils. Genital warts are transmitted through skin-to-skin contact during sexual activity with an infected person.
You can get genital warts even if you use condoms or engage in genital touching because condoms don’t cover all areas of skin where the virus can spread. You can also get genital warts from sharing sex toys with an infected person.
Genital warts can also potentially be spread if you touch yourself where there is an infected area and then touch another part of your body. Although rare, the virus can also be passed to a baby from its mother during birth.
We’ll explain how you might be able to tell if a woman has genital warts next. However, some people never develop symptoms even after contracting HPV, which makes it possible to pass the virus on without knowing you have it. About 70% of sexually active men and women are exposed to HPV during their lives, but very few experience noticeable symptoms.
If symptoms do appear, you might have one genital wart bump, or you could have several. They often look whitish or skin-colored. However, genital warts may also appear pink if they are new or red if they’ve become irritated. This is why many women mistake genital warts for common irritants like shaving bumps, ingrown hairs, or minor skin rashes.
It’s important to note that if your OBGYN has ever called to tell you that your pap smear revealed HPV, that doesn’t automatically mean you have genital warts. There are at least 100 different known strains of HPV; most have no symptoms, are easily cleared by your immune system, and go away on their own.
Only a couple of specific HPV strains cause genital warts, just like only certain strains of HPV are linked to cervical cancer. The strains of HPV that can cause cancer do not cause genital warts.
Learn about other STDs with our Ultimate Guide to STDs
Risk Factors for Developing Genital Warts
Genital warts are usually caused by specific strains of the human papillomavirus (HPV), which spreads through direct skin-to-skin contact during sexual activity. Here are the main factors that can increase your risk of developing genital warts:
Unprotected Sexual Activity
Engaging in sex without using condoms significantly increases the risk of HPV transmission. Although condoms provide a measure of protection, they do not fully eliminate the risk of transmitting genital warts.
Multiple Sexual Partners
Having multiple sexual partners increases your chances of being exposed to HPV. The more partners you have, the higher the risk of coming into contact with someone who has the virus, which might be a strain that causes genital warts.
Weakened Immune System
People with weakened immune systems are more at risk. Conditions like HIV or taking immunosuppressive medications can make it easier for HPV infections to take hold and for warts to persist or get worse.
Early Onset of Sexual Activity
Starting sexual activity at a young age also heightens the risk of contracting HPV. Younger individuals are more susceptible to being exposed to the virus early on.
It’s crucial to understand that while these factors increase the likelihood of developing genital warts, not everyone exposed to HPV will show visible symptoms. Some may carry the virus without any outward signs.
How Do You Tell If It’s a Genital Wart or Not?
Noticing a bump or sore on or around your genitals that wasn’t there before can be alarming, especially if you are sexually active and at higher risk of contracting genital warts or other STIs.
While genital warts have a few distinct features and symptoms, which we will discuss next, they can resemble other common skin conditions, such as razor burn or ingrown hairs. For this reason, searching online for genital warts images or wart disease images could lead to unnecessary stress.
If you are concerned about bumps on or around your genitals, only a medical professional, such as an OB-GYN, knows how to visually identify genital warts. A medical exam is the only way to confirm whether a bump is truly a genital wart or something else.
What Are The Symptoms Of Female Genital Warts
The symptoms of female genital warts can vary depending on the individual. The most well-known symptom is their unique appearance.
For starters, many ask if genital warts have pus. This is often one way to distinguish genital warts from other conditions. Unless a genital wart becomes infected, leading to a blister or sore, genital warts themselves do not typically produce pus. If you notice pus or fluid leaking from a bump, it’s more likely another type of infection or condition.
Most of the time, genital warts do not hurt when you touch them. Genital warts are usually painless; however, in some cases, they might itch, burn during urination, and cause vaginal pain, especially if there is friction.
Symptoms of genital warts are usually mild to moderate and may come and go over time. However, other potential symptoms can occur as a result of this common sexually transmitted infection. For example, genital warts may cause bleeding after sex. This symptom is less common than others, but it is still a possibility.
If you are experiencing these symptoms, you may have genital warts:
- Flesh-colored or grey growths around your vagina, anus, or upper thighs
- Cauliflower-like growths
- Growths that may be internal
- Itching or bleeding from your vagina or anus
- Changes to the flow of urine
Some people will carry the HPV virus that causes genital warts and never develop symptoms. They may never know they even have the genital warts virus without a screening from an OBGYN. If symptoms do occur, they may not appear for weeks, even years, after coming in contact with the virus.
What Do Genital Warts Look Like?
Genital warts can have a range of appearances, depending on factors such as the location and severity of the infection. As mentioned above, genital warts often appear as small, flesh-colored, or pink growths on the skin or mucous membranes in the genital area.
Genital warts can be raised or flat and have a rough or smooth texture, but they can also have a cauliflower-like appearance, with multiple small growths clustered together. In some cases, genital warts may be so small that they are not visible to the naked eye and are detected through a physical exam or Pap smear.
If you notice any unusual growths or changes in your genital area, it’s always best to see a healthcare provider for an accurate diagnosis and appropriate treatment. The red bumps on your but or genital bumps you see might be genital warts, but they could also be a common skin irritant.
What Can Be Mistaken For Genital Warts In Females?
Visually, several conditions may resemble genital warts. The appearance of genital warts is often mistaken for common skin conditions, such as shaving bumps, ingrown hairs, or a skin tag. Other lesser-known conditions can also resemble genital warts.
Distinguishing genital warts from other similar conditions can be challenging without professional help, and you should never attempt to self-diagnose a bump on or around your genitals.
That said, it can offer some peace of mind for those worried about a genital bump to have a better understanding of how to tell them apart from other skin conditions.
How to Differentiate Genital Warts from Other Skin Conditions
If you notice a bump around your genitals, it is always best to schedule an appointment with a doctor who can give you a more definitive answer and help you take any additional steps necessary. This guide is only to provide you with a better idea of what a bump or bumps on your genitals may or may not be.
Common Conditions Mistaken for Genital Warts:
- Skin Tags
- Appearance: Small, soft skin growths that look like a tiny deflated balloon on a stalk.
- Transmission: They are not sexually transmitted and are usually harmless.
- Molluscum Contagiosum
- Appearance: Viral infection causing small, round, flesh-colored bumps.
- Transmission: Can spread through direct skin-to-skin contact, similar to genital warts.
- Fordyce Spots
- Appearance: Tiny, raised, yellowish, or skin-colored spots found on the genitals or other body parts.
- Cause: Enlarged sebaceous glands, not linked to STIs.
- Seborrheic Keratosis
- Appearance: Noncancerous, warty growths that can be white, brown, or black, often with a “stuck-on” look.
- Prevalence: More common among older adults; not sexually transmitted.
Distinguishing Features
- Skin Tags: Typically painless and not prone to changes unless irritated.
- Molluscum Contagiosum: Tend to have a central dimple or indentation in the bump.
- Fordyce Spots: Consistent in appearance and usually do not change over time.
- Seborrheic Keratosis: Often develops a rough, bumpy texture and varies greatly in color.
What STIs Can Be Mistaken for Genital Warts?
Most common STIs, such as chlamydia or gonorrhea, do not typically cause visible bumps or growths on the skin. The two sexually transmitted infections that might slightly mimic genital warts are herpes and syphilis. However, they have very different characteristics and require distinct treatments.
- Herpes: Genital herpes often presents as painful, fluid-filled blisters rather than solid bumps. These blisters usually break open and form sores that eventually scab over. Genital herpes is not curable, but antiviral medications can reduce the severity and frequency of outbreaks and lower the risk of spreading the virus.
- Syphilis: Syphilis is a bacterial infection caused by the bacterium Treponema pallidum. It often begins as a firm, painless sore (called a chancre) that usually appears where the bacteria entered the body. If untreated, syphilis typically evolves to include a widespread rash, fever, swollen lymph nodes, and, in late stages, serious damage to organs and the nervous system. Syphilis is curable with the correct antibiotic treatment.
To the untrained eye, bumps on or around the genitals can look similar and cause unnecessary worry. An OB-GYN will easily be able to distinguish between genital warts and other infections, perform tests if needed, and recommend the proper treatment.
Importance of Professional Diagnosis
If you observe any unusual growths or changes in your genital area, consult a healthcare provider. They possess the expertise to differentiate between genital warts and other conditions accurately. Early diagnosis ensures you receive the appropriate treatment, whether it’s for genital warts or another condition.

How To Prevent Female Genital Warts
As genital warts are a sexually transmitted infection that can be passed from person to person through skin contact, they can be hard to prevent.
There is no sure way to prevent genital warts, and sexually active people are at risk, but there are several steps you can take to reduce your risk of exposure:
- Get vaccinated against HPV. The HPV vaccine is a very effective way to protect yourself against the virus that causes genital warts.
- Get regular screenings for HPV and other STIs for early detection and management of HPV-related conditions.
- Use condoms and dental dams every time you have sex or oral sex.
- If sharing sex toys, make sure they too are covered in a condom and washed between use.
- Avoid skin-to-skin contact with someone who has genital warts. (Remember that even after treatment, the virus can still be passed up to 3 months after warts have been removed.)
- Reduce the number of sexual partners to lower your overall risk of exposure to genital warts.
- Have open and honest communication with your partner(s) about your and their sexual health.
- If you are pregnant, there is a chance you could pass them to your baby. Seek guidance from your obstetrician.
Complications From Genital Warts
When properly diagnosed and treated, genital warts are usually manageable and may clear over time with the right care. However, leaving genital warts untreated or failing to address the underlying HPV infection can potentially cause complications.
Cervical Cancer Caused by HPV
Warts are typically caused by low-risk HPV strains, like HPV types 6 and 11, and do not cause cancer. However, some strains of HPV can cause cancer, and it is possible to be infected with more than one strain of HPV.
There are low and high-risk strains of HPV that might cause cervical cancer. The highest-risk HPV strains to cause cancer are HPV 16 and 18. These two strains are responsible for about 70% of cervical cancers.
Even though not all types of HPV infections cause cancer, you should still get a full check-up. Having HPV and other sexually transmitted infections can also make it easier to contract HIV. This is why it’s important for women to get screened regularly as part of a preventive health care routine.
Problems During Pregnancy
In rare cases, female genital warts can cause complications during pregnancy. If the warts are present in the birth canal, they can obstruct the baby’s passage during delivery. This obstruction can lead to the need for a cesarean section to avoid harm to the baby.
While female genital warts are not typically life-threatening, they can cause several complications that can impact a woman’s physical and emotional health.
To mitigate the risks of these complications, it is critical to practice safe sex and undergo regular STI testing to prevent the spread of HPV and detect any abnormal cell changes early on.
Urinary Obstruction
If the warts are near the urethra, they may grow and obstruct urine flow, leading to discomfort and pain during urination.
Female genital warts can sometimes grow near the opening of the urethra, which is the tube that carries urine from the bladder to the outside of the body.
When this happens, the growth of the warts can obstruct the flow of urine, leading to discomfort and pain during urination. The severity of the urinary obstruction can vary depending on the size and location of the warts.
Sometimes, the obstruction may be mild, causing slight discomfort or a weak urine stream. In more severe cases, the warts can completely block the flow of urine, leading to acute urinary retention, a medical emergency requiring immediate treatment.
How Are Female Genital Warts Treated?
While treatment for genital warts doesn’t eliminate the human papillomavirus (HPV) itself, if you have genital warts, the bumps themselves are treatable. In this section, several treatment options will be covered for female genital warts.
Treatment options include topical medications, cryotherapy (freezing), laser surgery, and electrosurgery. Some methods may be more effective than others, depending on the size and location of the warts. Visible warts on the outside of your body are easier to treat.
Below are detailed explanations of the mentioned treatments:
Cryotherapy for Female Genital Warts
Cryotherapy is a standard treatment for female genital warts. A healthcare provider uses liquid nitrogen to freeze and destroy the warts during this procedure.
The extreme cold causes the warts to peel off over time. Cryotherapy is often effective for small to medium-sized warts and is relatively quick and straightforward. However, complete removal may require multiple treatments.
Laser Surgery for Female Genital Warts
Laser surgery is another option for treating genital warts. This procedure uses a focused laser beam to vaporize and remove the warts. Laser surgery is precise and can target warts in delicate areas with minimal damage to surrounding tissue.
Laser surgery is often recommended for larger or hard-to-reach warts. Recovery time is typically shorter than other treatments but may require multiple sessions.
Electrosurgery for Female Genital Warts
Electrosurgery, or electrocautery, involves using an electrical current to burn and remove genital warts. This method can be effective for warts of various sizes and locations. It’s a quick procedure that cauterizes the warts, helping to stop bleeding and reduce the risk of infection.
However, there may be some discomfort during the process, and multiple sessions may be necessary for complete wart removal.
Topical Medications for Female Genital Warts
Topical medications can treat genital warts, especially in cases where warts are small and widespread. These medications typically contain chemicals that work to destroy the warts over time.
Some examples of topical treatments include:
- Podofilox: Podofilox is a gel or solution-based dosage available through a doctor’s prescription, used to treat warts between the genitals and rectum.
- Imiquimod: Imiquimod is a cream-based dosage available through a doctor’s prescription and applied to help your body fight the viruses that cause warts.
- Trichloroacetic acid (TCA): Trichloroacetic Acid (TCA) is a chemical solution applied by a professional healthcare provider that kills the proteins of genital wart cells.
Through repeated use, warts will gradually decrease in size and eventually disappear. Applying these medications requires strict adherence to a healthcare provider’s instructions, and visible results may take several weeks. Know that these treatments do not cure HPV infection.
Topical treatments are generally less invasive than cryotherapy, laser surgery, or electrosurgery.
Is Treatment Necessary for Genital Warts?
In most cases, treatment is unnecessary if your genital warts are small and you don’t have any severe symptoms. Moreover, genital warts are easier to treat if you begin treatment as soon as you notice them. You also may want to treat genital warts for cosmetic reasons, as they may be embarrassing.
During treatment, avoid irritating soaps and lotions. Having intercourse may also irritate the skin, and it is best to avoid that until treatment is finished. It may take several weeks for a genital wart treatment to be effective, depending on the type of treatment.
Remember, genital warts are different from warts on the hand or feet. Do not try an over-the-counter remedy for these areas, or attempt to remove warts from the genital area yourself. This could damage the delicate skin in the genital region.
Dr. Lodge, an experienced OBGYN in Cool Springs, can prescribe the best course of treatment that won’t harm your skin.
Can Genital Warts Recur After Treatment?
Yes, genital warts can recur even after treatment. The primary reason for this is the persistence of the human papillomavirus (HPV) in the body. Although treatments can remove visible warts, they don’t eliminate the virus entirely.
How to Manage the Recurrence of Genital Warts
- Regular Follow-Ups: It’s crucial for individuals who have had genital warts to schedule regular check-ups with their healthcare providers. This helps in the early detection and management of any recurring warts.
- Preventive Measures: Adopting preventive strategies, such as using barrier protection during sexual activities, can significantly reduce the risk of recurrence.
- Healthy Lifestyle: Maintaining a robust immune system through a healthy lifestyle, including a balanced diet, regular exercise, and avoiding smoking, can help the body fight off HPV more effectively.
While genital warts can recur, taking proactive measures and working closely with healthcare providers can help manage and reduce the risk.
Can Female Genital Warts Be Cured?
The good news is that warts themselves can be treated and removed. Some cases of genital warts will resolve on their own over time, but they cannot be guaranteed to go away entirely without treatment.
Unfortunately, there is no medical cure for the human papillomavirus (HPV) itself. Some people’s bodies are able to clear the virus naturally over time. You will need screenings to confirm if the virus is still active in your body.
There is no such thing as a mild case of genital warts in men or women. If you see the wart or have tested positive for the virus, you have the STI and may be able to transmit it.
How Do I Confirm if I Have Genital Warts?
Noticing a new bump in your genital area can be unsettling, especially if you’re unsure what it is. Because genital warts can look like many other harmless skin conditions, the only way to know for sure is to have a proper physical examination and testing by your gynecologist.
What to Expect During a Medical Exam and Testing For Female Genital WartsDuring your exam, you may be asked a few questions about your symptoms and sexual history.
Next, Dr. Lodge will perform a pap smear to test for the Human papillomavirus that causes genital warts. A Pap test checks for abnormalities of cancer in cells collected from your cervix, and an HPV test will be done at the same time.
To check for warts themselves, Dr. Lodge can identify them visually on the exterior and interior of the genitals. He will also check for hidden warts inside the vagina. This process should not be painful. Dr. Lodge handles screenings like this regularly.
Schedule a Screening for Genital Warts in Cool Springs, Tennessee
If you are experiencing any of the symptoms associated with female genital warts, it is important to seek medical treatment as soon as possible. It is also important for women who are sexually active to be screened for HPV on a regular basis, especially if they have multiple sexual partners.
Please give the staff at Cool Springs OBGYN in Brentwood, Tennessee, a call to make an appointment. Call us at 615.690.6600, Monday through Thursday, for women’s health care with all the latest advances in gynecology.

