If you are experiencing unexplained bleeding, heavy or inconsistent menstrual periods, or unusual discharge, uterine polyps aren’t typically the first cause to come to mind.
Uterine polyps, also known as endometrial polyps, are not a condition most women are familiar with, but they aren’t rare. Up to 3 in 10 women will have uterine polyps at some point in their lives, mainly in women over 30 and those nearing menopause or post-menopausal.
Small polyps may cause no symptoms and can go away on their own; however, in many instances, minimally invasive surgery is required to remove the polyps.
While they can bring discomfort and might require surgical removal, the good news is that most (approximately 95%) of uterine polyps are noncancerous (benign.)
In this article, we will go over what uterine polyps are, what causes them, symptoms you might experience, how they are diagnosed, problems uterine polyps can cause if left untreated (which includes infertility), and surgical removal options should you be diagnosed.
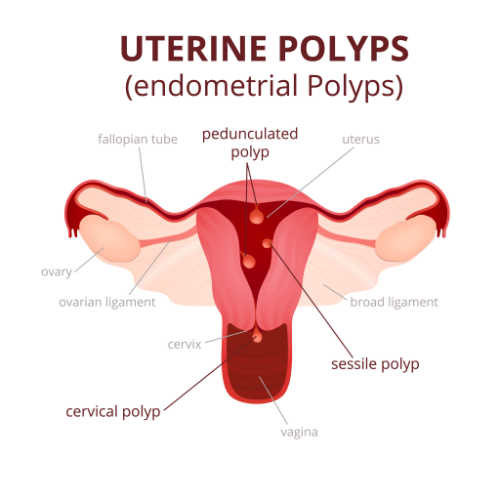
What Are Uterine Polyps?
Uterine polyps, also known as endometrial polyps, are fleshy growths that develop along the inner wall of the uterus and extend into the uterine cavity.
Typically, uterine polyps are very small (less than 1cm) but can be as large as a golf ball. You may have only one polyp or multiple polyps at once.
Some uterine polyps don’t need treatment, but doctors have several ways to safely remove polyps if they require attention.
What Causes Uterine Polyps?
The overgrowth of cells in the lining of the uterus (endometrium) leads to the formation of uterine polyps. Still, the exact cause and risk factors for this overgrowth are not fully known.
However, because it is rare for uterine polyps to develop before the onset of a woman’s menstrual period, it is believed they are affected by hormone levels, specifically in response to the presence of estrogen in the blood.
Overexpression of estrogen and progesterone receptors, endometrial aromatase, and mutation in the HMG1C and HMGI(Y) genes have also been associated with uterine polyps.
Obesity and Uterine Polyps
Regarding risk factors, there is some proof that obesity can increase your chance of developing uterine polyps. This is because obesity increases the levels of estrogen in the blood.
Tamoxifen therapy is another risk factor for the development of uterine polyps. As many as 36% of postmenopausal women treated with tamoxifen develop uterine polyps.
What Are The Symptoms of Uterine Polyps?
Many women who have uterine polyps show no symptoms. If symptoms are present, one or more of the following might occur:
- Irregular menstrual periods (can’t predict their timing, length, or heaviness.)
- Bleeding or spotting between menstrual periods
- Excessively heavy menstrual periods
- Abnormal vaginal discharge
- Vaginal bleeding after menopause
If you have one or more of the symptoms above, it’s important to see a doctor. They can help determine whether you have uterine polyps or another condition causing similar symptoms.
How Are Uterine Polyps Diagnosed?
If a woman is displaying symptoms of uterine polyps, they are typically diagnosed by a procedure called a hysteroscopy. During a hysteroscopy procedure, a thin telescope is inserted into the uterine cavity, allowing the doctor to see inside the uterus.
Hysteroscopy
A hysteroscopy is the most accurate method for diagnosing uterine polyps and the most common procedure used to remove uterine polyps, which we will discuss further down.
Ultrasound
An ultrasound scan is another way doctors can detect a uterine polyp. However, an ultrasound can result in false positives or require further diagnostic testing, especially in younger women still having menstrual periods. This is because the thickened fold of the uterus lining can easily be interpreted as polyps on an ultrasound scan.
Hysterosalpingography
Occasionally, hysterosalpingography, or HSG, is used to diagnose uterine polyps. During this procedure, a special x-ray of the uterus is taken after filling it with a dye.
Whatever procedure is used, your doctor will also take a tissue sample from the polyp and send it to a lab to rule out cancer.
Are Uterine Polyps Dangerous?
Uterine polyps are relatively common and are rarely cancerous. However, some precancerous changes in the uterus and uterine cancers can first appear as uterine polyps.
For this reason, if you have uterine polyps, your doctor will likely recommend removal of the polyp and will send a tissue sample for lab analysis to ensure the polyp is benign. If the tissue sample reveals your uterine polyp contains cancerous cells, your doctor will talk with you about the next steps.
Again, most uterine polyps are not cancerous or considered dangerous. That said, if left untreated, they can cause issues such as:
- Heavy bleeding
- Pain
- Infertility in premenopausal people
- Postmenopausal bleeding
Even though uterine polyps are rarely cancerous and severe complications from uterine polyps typically do not occur, it is always best to take a proactive approach if you are experiencing any symptoms or are at high risk for uterine cancer.
How Do Uterine Polyps Cause Infertility?
Uterine polyps could very well be one reason a woman has difficulty becoming pregnant. In fact, it is often during the process of In Vitro fertilization (IVF) that many women discover they have uterine polyps.
There are several reasons uterine polyps could cause infertility or make conceiving more difficult. Uterine polyps can potentially…
- Act like an intrauterine device (IUD) by preventing an embryo from implanting in the uterus.
- Cause local inflammation in the uterine lining.
- Cause interference with sperm transportation
- Produce something called glycodelin, which has been shown to cause the uterine lining to become less receptive to implantation.
It is possible to still become pregnant, even if you have polyps in your uterus. There is also no guarantee that you will conceive after polyp removal. However, some studies suggest higher pregnancy rates in women who undergo hysteroscopy polyp removal.
What Is The Best Treatment For Uterine Polyps?
Small polyps without symptoms may resolve on their own. In this case, surgery might not be required. Instead, your doctor might suggest they monitor the polyps over time.
However, if symptoms are present, it is suggested that the polyps be removed and evaluated to confirm no evidence of cancer. Removal of polyps is also advised in all postmenopausal women and all women at high risk for uterine cancer, even if no symptoms are present.
If your uterine polyps need to be removed, it is typically done through a hysteroscopy procedure, which is the same procedure often used to diagnose uterine polyps, only this time, one extra step is performed to remove the polyps (a polypectomy.) You might also have an accompanying endometrial ablation procedure.
Here is what to expect from both procedures.
Hysteroscopy Procedure
A hysteroscopy procedure, sometimes called a polypectomy with hysteroscopic excision, is a minimally invasive outpatient procedure that does not usually require anesthesia.
Typically, only a topical local anesthetic numbing cream is used to numb your cervix during the procedure to help with the moderate cramping the procedure can cause. A mild sedative might also be used.
During the short in-office procedure, your doctor will insert a speculum into your vagina to hold it open. Next, a long, thin tube with a light and camera, called a hysteroscope, is passed into your womb and through your cervix. This is the point in the procedure where you might experience some cramping and discomfort. If it becomes too much, your doctor can stop at any time.
A fluid is then gently pushed into the womb to make it easier for your doctor to see. A camera sends pictures to a monitor allowing your doctor to spot the abnormalities. The polyps are then removed using surgical scissors, forceps, a laser, or another electrical device.
Last, your doctor will administer silver nitrate to help stop any bleeding. The polyp is then sent to a lab for testing to confirm whether it is benign or cancerous. Again, uterine polyps are rarely cancerous.
If you were not put to sleep, you will be able to go home on the same day as the procedure. If you have a more complicated polypectomy, you’ll be in a recovery room until you wake up from the anesthesia and might need to stay in the hospital for a day or two.
You might need to take it easy for a day or two, but you can generally return to normal activities the following day if only a local anesthetic was used and within a few days if it was a more complicated hysteroscopy.
Endometrial Ablation
Sometimes, if heavy bleeding is a concern, another minimally invasive procedure called endometrial ablation is performed in conjunction with removing uterine polyps.
Endometrial ablation removes the endometrium, which is the lining of the uterus. There are different types of endometrial ablation. If this procedure is needed, your doctor will discuss which of the following removal methods is best for your unique situation.
- Hydrothermal: Fluid is gently pumped into your uterus and then heated, destroying the uterine lining.
- Balloon therapy: A thin tube with a special balloon is placed into your uterus. Heated fluid fills the balloon, which then expands and destroys the uterine lining.
- High-energy radio waves: Electrical mesh is placed and expanded in your uterus. Energy and heat are then sent by strong radio waves damaging the lining, which is then removed via suction.
- Freezing: This is one of the more commonly used methods for endometrial ablation. It is often referred to as “cryoablation.” During the short procedure, a probe with a cold tip freezes off the lining of your uterus.
- Microwave: A slender wand is inserted through the cervix. The wand emits “microwave energy,” which heats the endometrial tissue and destroys it.
Post Uterine Polyp Removal
Once removed, uterine polyps can recur. In that case, you might need to undergo treatment more than once.
If the polyps are found to contain precancerous or cancerous cells, removal of the uterus (a hysterectomy) may be necessary.
Hormonal medications might also be prescribed.
Where To Get Help If You Have Uterine Polyps
Cool Springs Obstetrics and Gynecology has been providing quality women’s health care for over 20 years to women of all ages all across Cool Springs, Downtown Franklin, Brentwood, and surrounding areas in Williamson County.
Dr. Lodge and his team of board-certified doctors, nurse practitioners, medical assistants and nurses have excellent experience with all women’s health issues, including uterine polyp diagnosis, treatment, and removal.
We are currently accepting new patients. Call us at 615-690- 6600 to book your appointment, or ask our friendly staff any questions you might have about uterine polyps or any other women’s health concerns.

